Radiotherapy for children
If your child is diagnosed with a brain tumour, they may receive radiotherapy as a treatment. This uses controlled and targeted doses of high energy beams of charged particles to destroy the tumour cells, whilst causing as little damage as possible to surrounding healthy cells.
On this page:
- Will my child have radiotherapy?
- What happens during radiotherapy?
- What happens when my child is given radiotherapy?
- What are the side-effects of radiotherapy?
- Frequently Asked Questions
- If radiotherapy doesn’t work
Will my child have radiotherapy?
Not all children diagnosed with a brain tumour will have radiotherapy.
There are two main reasons why your child may have radiotherapy:
- if your child’s tumour cannot be operated on.
- after surgery to destroy any remaining tumour cells, and so lower the chances of the tumour returning.
The decision to give radiotherapy will be based on a number of factors:
- your child’s age
- location of their tumour
- type and size of their tumour
- other factors e.g. whether the tumour is growing or causing symptoms.

Join our community on Facebook
Our closed Facebook group for parents is a great place to connect with other parents affected by a brain tumour and share your experiences.
If your child is under three years old, it is unlikely that they will have radiotherapy. Radiotherapy can be damaging to very young children, having a long-term impact on cognition, growth and hormone levels. However, with some tumour types e.g. ependymoma, younger children may have treatment with radiotherapy, if the tumour is in the posterior fossa (the back of the skull).
At all times the type and dose of radiation needed for treatment will be taken into account and the benefits of treatment will be weighed against any immediate or long-term risks.
Your child may also have radiotherapy alongside chemotherapy for some tumour types.
What happens when my child is given radiotherapy?
Before treatment
Planning
A team of medical specialists very carefully plan your child’s radiotherapy treatment to ensure that it reaches as many tumour cells as possible, whilst avoiding as much healthy tissue as possible.
First a ‘radiotherapy planning scan’ will be taken. This is usually a CT scan, but sometimes an MRI scan. The scan creates a 3D image of your child’s tumour, showing its shape and location in the brain. This image and measurements from the scan allow more precise planning of where the radiotherapy needs to be targeted, the dose required and how often it needs to be given.
Health professionals will make all efforts to avoid areas of the brain where irradiation (giving radiotherapy) may lead to long-term problems.
These areas include the brain stem (responsible for functions such as breathing and heart rate); the optic nerve (which helps you see); the hormone producing area; and the cochlear in the ear (to reduce longterm hearing loss).
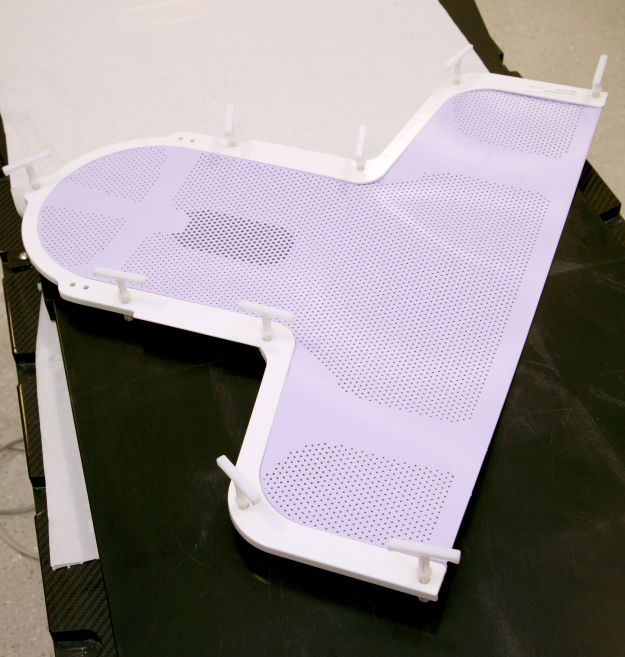
It is important that your child lies very still during treatment, so that medical experts may be able to direct the radiotherapy to the correct part of the brain. To help your child stay still, medical staff will fit your child with a treatment mask designed specifically for their face and head. This mask fixes to the treatment couch to keep their head still and in the same place each time they have treatment.
There are different types of masks, made from different materials. The manufacturers make these masks by smoothing the warmed material onto your child’s face, so that the final mask is an exact replication of the size and shape of their head. Gaps are left for the eyes, nose and mouth, so your child is always able to breathe easily.
A play therapist may work with your child to make wearing the mask less daunting. They can also arrange for your child to look at a radiotherapy machine before their treatment so that they are mentally ready when they begin treatment.




Treatment
The medical team plan your child’s treatment to suit their individual needs, so may be very different to the treatment of other children you may meet.
If your child is very young or extremely anxious and won’t keep still, doctors will give them a short general anaesthetic. Or a health play specialist may work with your child to keep them calm and still.
- Your child will lie on the radiotherapy bed with the radiotherapy machine above them
- Medical staff will place the mask over your child’s head and attach it to the bed, taking some time to position them.
- Medical staff will leave the room before switching the radiotherapy machine on, but remain nearby. They will be able to see, hear and speak to your child, should they need them.
- Your child won’t be able to see or feel the radiotherapy beams nor feel any heat from it. They will be able to hear the machine.
- Once the treatment session, called a ‘fraction’ is finished, medical staff will go back into the room, remove the mask and help your child off the bed.
- The medical staff will keep your child’s mask until the next treatment session.
How long will treatment take?
Treatment times will vary, depending on your child’s individual treatment plan.
However, each treatment session (fraction) generally only lasts a few minutes. The treatment appointment will be considerably longer, due to the time taken to position your child in the correct place. If you child is having radiotherapy to their spine (known as craniospinal radiotherapy), this can also take longer.
A typical radiotherapy plan is once a day, Monday to Friday, with a break at the weekends.
It is common for your child to have radiotherapy for 4 to 6 weeks.
Your child’s health team can tell you your child’s exact treatment plan.
After treatment
If your child is having radiotherapy as an outpatient, they will be able to go home after each session. If they need to remain in hospital for another treatment, a nurse will take them back to their ward.
After the whole course of treatment, your child will have regular check-ups to monitor the effects of the radiotherapy on the tumour and any side-effects you child may get.
It is likely they will experience some side-effects. Some of these will be temporary and gradually clear once the treatment has finished. Others may be long-term.
What are the side-effects of radiotherapy?
These will partly depend on the area of the brain where your child receives the radiotherapy, and what that area controls. Also radiotherapy works best on rapidly dividing cells, such as tumour cells, but some normal cells in the treatment area also divide rapidly, so these areas tend to have the most common side-effects. These include hair and skin cells. Read more about the side-effects of radiotherapy.
Frequently Asked Questions
-
It is highly likely that your child will need to take some time out of school during the course of their radiotherapy treatment.
This may be due to tiredness, other side-effects or for daily trips to the hospital.
The Brain Tumour Charity has produced some education resources to help them get the support they need to minimise the impact on their school/college work and keep up their friendships during treatment.
-
No, your child won’t be able to see or feel the radiotherapy beams and they won’t feel any heat from it either.
They will hear the machine though. It may be helpful to talk about this with your child before they have treatment so that they know to expect it and are not afraid. The Brain Tumour Charity animation about radiotherapy for children includes a sample of the noise.
A health play specialist can also help your child become used to the sounds of the machine.
There have been some cases where children have said they have been aware of a strange smell during radiotherapy.
-
No. The radiation comes from the machine and will not stay inside your child’s body. Once they leave the hospital it is safe for them to be around other people, including their brothers and sisters and other children.
-
If your child is under 3 years old, it is unlikely that they will have radiotherapy.
Radiotherapy affects some normal brain cells around and beyond the tumour. With adults many of these cells can recover, though they can still result in side-effects.
However, the brains of children are still developing and those under 3 years still have much developing to do. Radiotherapy can interfere with this development, causing serious long-term side-effects – for example on cognitive development (thinking), physical development and/or hormone levels.
Despite this, some tumour types e.g. ependymoma, may be treated with radiotherapy in younger children if the tumour is in the posterior fossa (the back of the skull cavity).
If your child is under three and their health team recommend radiotherapy, make sure they talk through the reasons for this decision with you.
If radiotherapy doesn’t work
Although healthcare professionals carefully develop your child’s treatment plan to be as effective as possible while having the fewest risks or side-effects, sometimes radiotherapy may not work. This can be worrying, but just because one treatment hasn’t worked, it doesn’t mean others won’t.
Find out more about what happens when treatment doesn’t work.
Radiotherapy for children – Standard format (pdf) –
Find out more about Radiotherapy for children in the full fact sheet – including more information about the longer-term effects and on resources to deal with hair loss.
Radiotherapy for children – Clear print (pdf) –
Find out more about Radiotherapy for children in the full fact sheet – Clear print version, designed to RNIB guidelines. Includes more information about the longer-term effects and on resources to deal with hair loss.
Support and Information Services
Research & Clinical Trials Information
You can also join our active online community.
In this section

Get support
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading

Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.

Radiotherapy for children
Dr Gillian Whitfield, Consultant Clinical Oncologist, The Christie, Manchester, talking at our National Paediatric Information Day.
