Glioblastoma treatment
The recognised glioblastoma treatment currently is surgery to remove as much of the tumour as possible, followed by a combination of chemotherapy and radiotherapy.
But, there are other treatment options available, as well as new developments in the established treatments. On this page we’ll look at some of these methods for treating glioblastomas.
Glioblastoma treatments include:
Surgery as a glioblastoma treatment
The first treatment for glioblastomas is usually neurosurgery. Your surgeon will try to remove as much of the tumour as possible. This is known as debulking.
With glioblastomas it can be difficult to remove the whole tumour because:
- they are diffuse, this means they have threadlike elements that spread out into the brain
- it can be hard to tell the difference between the edges of the main part of the tumour and normal brain tissue.
This means that parts of the tumour may get left behind after surgery.
However, the development of 5-ALA is aimed at helping this. You can learn more about this ‘Pink Drink’ below.
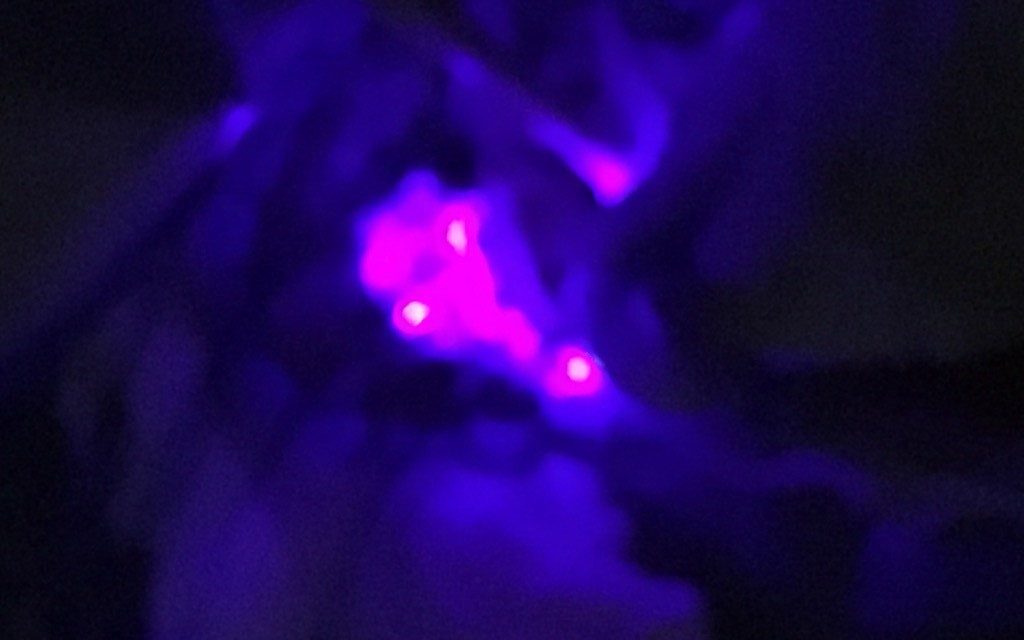
5-ALA: The Pink Drink
The Pink Drink causes tumour cells to glow bright pink under UV light and can be taken before surgery to help surgeons avoid healthy cells while removing more of the tumour.
Treating glioblastomas with chemoradiation
Chemoradiation comprises radiotherapy over a period of weeks along with rounds of the chemotherapy drug temozolomide (TMZ). It is used to slow the growth of any tumour cells that cannot be removed by surgery.
Temozolomide works by stopping tumour cells from making new DNA (the material that carries all their genetic information). If they cannot make DNA, they cannot divide into new tumour cells, so the tumour cannot grow. It is also thought to make the tumour cells more sensitive to the radiation.
Temozolomide is usually taken for a further six months after radiotherapy finishes.
A new development in glioblastoma treatment is DCVax-L. Adding this to chemotherapy might prolong the life of people affected by glioblastomas. You can read more about this trial below.

Trial finds DCVax-L® can prolong the lives of those living with a Glioblastoma
A major phase III clinical trial has found that novel treatment DCVax-L can prolong the lives of people diagnosed with a new or recurrent glioblastoma
Gliadel® wafers
Gliadel wafers are small wafers, coated with the chemotherapy drug carmustine. They are put directly into the brain at the end of surgery. This means the treatment gets around the blood-brain barrier that prevents many chemotherapy drugs from entering the brain.
The wafers are only licensed in the UK for use in recurrent glioblastomas (glioblastomas that have come back) and when the surgeon is confident that at least 90% of the tumour has been removed. Find out more about chemotherapy.
Avastin®
You may have heard that the use of another drug, called bevacizumab (Avastin), may be helpful in treating glioblastomas. This is a type of monoclonal antibody that aims to block the signals that help tumour cells grow.
However, in Europe it is felt that there is insufficient evidence for its effect on brain tumours and for this reason it is not licensed for use with brain tumours in the UK.
That being said, there may be ways that you can access it. You can learn more on our bevacizumab (Avastin) page.
Effectiveness of glioblastoma treatment
Unfortunately glioblastomas are aggressive tumours and often appear resistant to treatment. This is probably due to the fact that the cells within the tumour are not all of the same type. This is known as ‘heterogeneity’. This means that treatments will kill off some types of cell within the glioblastoma, but leave others, which can then continue to grow.
However, some of the research into the genes, which play a role in glioblastoma (GBM) development and growth, are starting to give us information about who may respond better to certain treatments. For example biomarker tests, such as:
- MGMT gene methylation test
This shows how likely you are to respond to the chemotherapy drug, temozolomide. - Mutations in the IDH-1 and TERT gene
These mutations are associated with effects on overall survival.
Many centres routinely test for these gene mutations, but if your hospital does not and you would like to have a test, ask your neuro-oncologist for information and advice about whether you are suitable.
Support and Information Services
Research & Clinical Trials Information
You can also join our active online community.
In this section

Get support
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading

Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.