Different types of brain tumour
There are more than 130 known types of brain tumour. These can be high grade (cancerous) or low grade (non-cancerous).
We’ve listed the different types of brain tumour below, with links where we have further information. This list is based on the World Health Organisation’s (WHO’s) latest classification of brain and central nervous system (CNS) tumours.
-
Brain tumours are classified according to the WHO guidelines. These take into account microscopic structure, biomarkers (explained below), and the grade of brain tumour.
Brain tumour grades are between 1 and 4. Grades 1 and 2 (low grade) are seen as non-cancerous and grades 3 and 4 (high grade) are seen as cancerous.
Biomarkers
Biomarkers are certain molecules or gene changes. These can give your healthcare team more information about your tumour, how it’s likely to respond to a treatment and how it’s likely to progress.
These are important because, for the first time, WHO classification defines tumours by their molecular features, not just what the tumour looks like under a microscope (histology).
Visit our biomarkers page to learn more about them and find more about getting a biomarker test.
What does NOS mean?
NOS stands for ‘not otherwise specified’. This designation is given when either:
- the hospital where you have your diagnosis doesn’t have the facilities to do a molecular analysis of your tumour, or
- the molecular analysis has been inconclusive.
Click below to find out more about the different types of brain tumour
- Astrocytomas
- Ependymoma
- Other gliomas
- Embryonal tumours
- Germ cell tumours
- Histiocytic tumours
- Melanocytic tumours
- Mesenchymal
- Neuronal and mixed neuronal-glial tumours
- Oligodendrogliomas
- Oligoastrocytomas
- Choroid plexus tumours
- Meningiomas
- Metastatic tumours
- Pineal region tumours
- Pituitary tumours
- Tumours of the nerves of the brain and spine
- Tumours of the sellar region
-
Astrocytomas are the most common type of primary brain tumour within the group known as gliomas. Primary means the tumour started in the brain instead of spreading from elsewhere. Astrocytomas grow from a type of brain cell called an astrocyte.
- Pilocytic astrocytoma
- Subependymal giant cell astrocytoma
- Pleomorphic xanthoastrocytoma
- Diffuse astrocytoma, IDH-mutant
- Diffuse astrocytoma, IDH-wildtype
- Diffuse astrocytoma, NOS
- Anaplastic astrocytoma, IDH-mutant
- Anaplastic astrocytoma, IDH-wildtype
- Anaplastic astrocytoma, NOS
- Anaplastic pleomorphic xanthoastrocytoma
- Glioblastoma, IDH-wildtype
- Glioblastoma, IDH-mutant
- Glioblastoma, NOS
- Diffuse midline glioma (formerly called DIPG), H3 K27M-mutant
Find out more information about astrocytomas, diffuse midline gliomas and glioblastomas.
-
Oligodendrogliomas are the third most common type of glioma. They grow from a type of brain cell which scientists call an oligodendrocyte. About 2-5% of all primary brain tumours are oligodendrogliomas.
- Oligodendroglioma, IDH-mutant and 1p/19q-codeleted
- Oligodendroglioma, NOS
- Anaplastic oligodendroglioma, IDH-mutant and 1p/19q-codeleted
- Anaplastic oligodendroglioma, NOS
-
Ependymomas are a type of glioma, and are most commonly found in children. They are the third most common childhood brain tumour. These tumours grow from ependymal cells, which line the ventricles of the brain (the fluid-filled spaces in and around the brain).
- Myxopapillary ependymoma
- Subependymoma
- Ependymoma
- Ependymoma, RELA fusion-positive
- Anaplastic ependymoma
Find out more about ependymomas.
-
Oligoastrocytomas are tumours that have characteristics of both oligodendrogliomas (from oligodendrocytes) and astrocytomas (from astrocytes). They used to be classified as ‘unspecified’ or ‘mixed’ gliomas.
- Oligoastrocytoma, NOS
- Anaplastic oligoastrocytoma, NOS
-
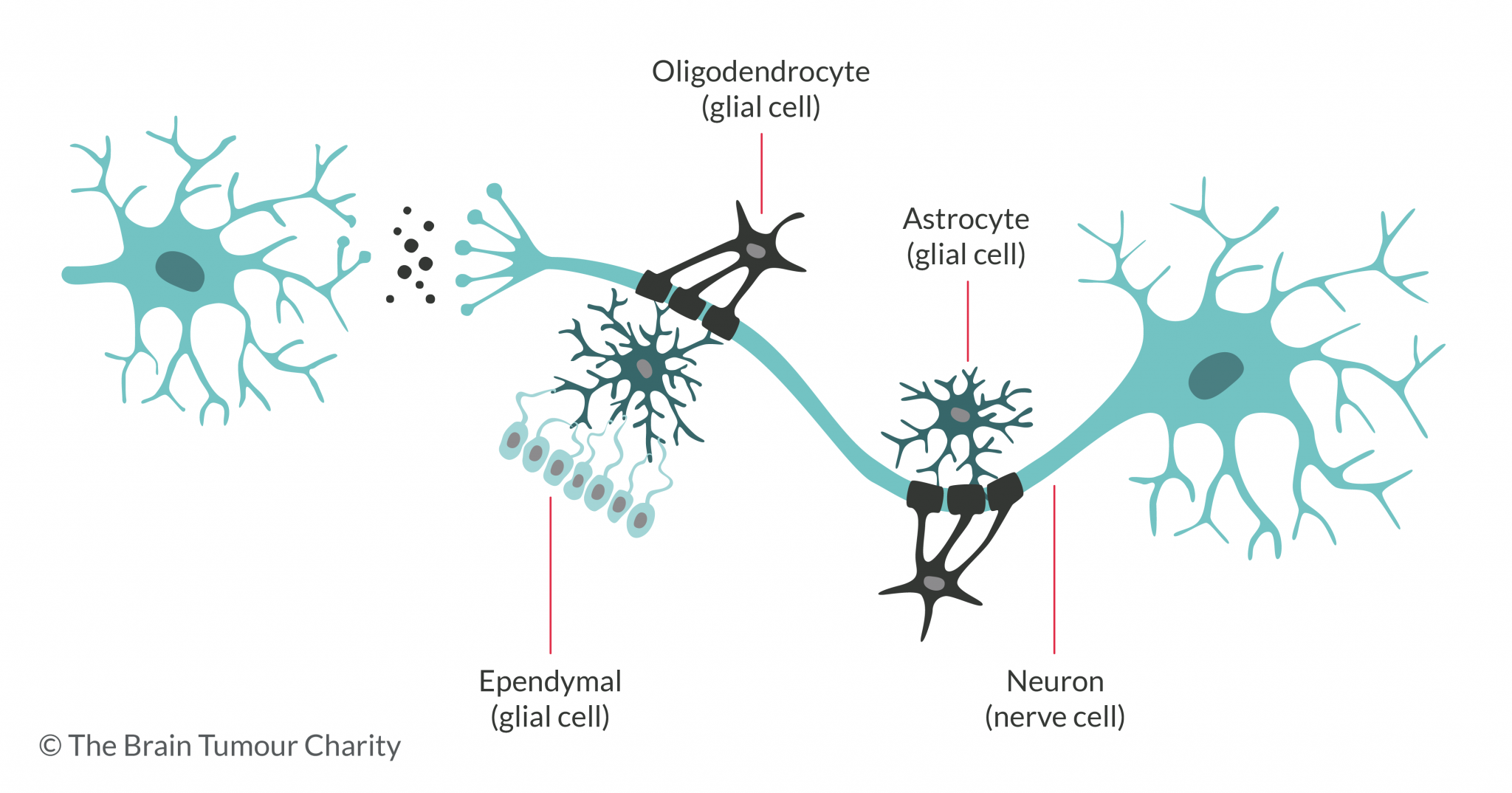
Gliomas grow from a type of brain cell called a glial cell. There are different types of glial cell, the main ones being astrocytes, oligodendrocytes and ependymal cells. Astrocytomas, oligodendrogliomas and ependymomas form from these cells. But there are other, rarer types of glioma.
- Angiocentric glioma
- Astroblastoma
- Chordoid glioma of the third ventricle
-
Choroid plexus tumours grow within the ventricles of the brain. They can block the cerebro-spinal fluid (CSF) from circulating and draining, causing pressure to build up in the skull.
- Choroid plexus carcinoma
- Choroid plexus papilloma
- Atypical choroid plexus papilloma
-
Embryonal tumours, previously known as primitive neuro-ectodermal tumours (PNETs), develop from cells left over from the earliest stages of our development – the embryonal stages. Nearly three-quarters (73%) of embryonal tumours are medulloblastomas.
- Atypical teratoid/rhabdoid tumour
- CNS embryonal tumour with rhabdoid features
- CNS embryonal tumour, NOS
- CNS ganglioneuroblastoma
- CNS neuroblastoma
- Embryonal tumour with multi-layered rosettes, C19MC-altered
- Embryonal tumour with multi-layered rosettes, NOS
- Medulloepithelioma
Medulloblastomas, genetically defined
- Medulloblastoma, WNT-activated
- Medulloblastoma, SHH-activated and TP53-mutant
- Medulloblastoma, SHH-activated and TP53-wildtype
- Medulloblastoma, non-WNT/non-SHH
Medulloblastomas, histologically defined
- Medulloblastoma, classic
- Medulloblastoma, desmoplastic/nodular
- Medulloblastoma with extensive nodularity
- Medulloblastoma, large cell/anaplastic
- Medulloblastoma, NOS
-
Germ cell tumours grow from germ cells – cells that are involved in our growth when we’re developing in the womb. Most germ cell tumours grow outside the brain, but those that grow in the brain usually occur in the area near the pituitary gland and pineal gland, at the base of the brain.
- Choriocarcinoma
- Embryonal carcinoma
- Germinoma
- Mixed germ cell tumour
- Teratoma
- Teratoma with malignant transformation
- Yolk sac tumour
-
Histiocytes are a type of cell that make up part of the immune system. Histiocytic diseases happen when there’s an over-production of these cells, which can lead to organ damage and the formation of tumours.
- Erdheim-Chester disease
- Histiocytic sarcoma
- Juvenile xanthogranuloma
- Langerhans cell histiocytosis
- Rosai-Dorfman disease
-
Lymphoma is a type of cancer in which white blood cells start growing uncontrollably. The lymph system, which includes tissues and organs, is responsible for making, storing, and transporting these white blood cells. Its primary job is to help the body to fight infections.
-
Melanocytes are cells that produce melanin, which is, the pigment that gives our skin its colour. Melanocytes are found in various places in the body, including in the meninges, the membranes that cover the brain. Very rarely, tumours can grow from the melanocytes in the meninges.
- Meningeal melanocytoma
- Meningeal melanocytosis
- Meningeal melanoma
- Meningeal melanomatosis
-
Meningiomas grow in the set of three membranes (meninges) that cover and protect the brain and also the spinal cord just inside the skull. Almost a quarter of all brain tumours in adults are meningiomas.
- Meningioma
- Anaplastic (malignant) meningioma
- Angiomatous meningioma
- Atypical meningioma
- Chordoid meningioma
- Clear cell meningioma
- Fibrous meningioma
- Lymphoplasmacyte-rich meningioma
- Meningothelial meningioma
- Metaplastic meningioma
- Microcystic meningioma
- Papillary meningioma
- Psammomatous meningioma
- Rhabdoid meningioma
- Secretory meningioma
- Transitional meningioma
-
Mesenchymal tumours arise from connective tissue. Connective tissue supports and connects the body’s organs, and is also found in the joints. If mesenchymal tumours are cancerous (malignant), they are called soft tissue sarcomas. Additionally Mesenchymal tumours may occur in the central nervous system and brain.
- Angiolipoma
- Angiosarcoma
- Benign fibrous histiocytoma
- Chondroma
- Chondrosarcoma
- Desmoid-type fibromatosis
- Epithelioid haemangioendothelioma
- Ewing sarcoma/PNET
- Fibrosarcoma
- Haemangioblastoma
- Haemangioma
- Hibernoma
- Inflammatory myofibroblastic tumour
- Kaposi sarcoma
- Leiomyoma
- Leiomyosarcoma
- Lipoma
- Liposarcoma
- Myofibroblastoma
- Osteochrondroma
- Osteoma
- Osteosarcoma
- Rhabdomyoma
- Rhabdomyosarcoma
- Solitary fibrous tumour / haemangiopericytom
- Undifferentiated pleomorphic sarcoma / malignant fibrous histiocytoma
-
A metastatic or secondary brain tumour is a tumour that started somewhere else in the body (such as the lung) and then spread to the brain. While a primary brain tumour is a tumour that started in the brain.
-
These tumours are rare and mostly non-cancerous. Most brain and central nervous system tumours grow from glial cells (see above). But neuronal tumours grow from neurons, a type of nerve cell that sends messages to and from the brain. Mixed neuronal-glial tumours grow from abnormal neurons and glial cells.
- Anaplastic ganglioglioma
- Central neurocytoma
- Cerebellar liponeurocytoma
- Desmoplastic infantile astrocytoma and ganglioglioma
- Diffuse leptomeningeal glioneuronal tumour
- Dysembryoplastic neuroepithelial tumour
- Dysplastic cerebellar gangliocytoma (Lhermitte-Duclos disease)
- Extraventricular neurocytoma
- Gangliocytoma
- Ganglioglioma
- Papillary glioneuronal tumour
- Paraganglioma
- Rosette-forming glioneuronal tumour
-
Tumours in the pineal region are rare. The pineal region is the area around the pineal gland. This gland sits behind the brain stem, in the centre of the brain. It produces melatonin, a hormone that controls sleep.
- Papillary tumour of the pineal region
- Pineal parenchymal tumour of intermediate differentiation
- Pineoblastoma
- Pineocytoma
-
Pituitary tumours, sometimes called pituitary adenomas, develop from the tissue of the pituitary gland. The pituitary gland is at the base of the brain. It controls other glands in the body, which in turn control many of the body’s functions.
-
These are tumours that grow from the nerves coming from the brain (cranial nerves) and spine (spinal nerves). The most common type of cranial nerve tumour is a vestibular schwannoma (sometimes called an acoustic neuroma). Specifically it affects the nerve that runs from the brain to the ear.
- Hybrid nerve sheath tumours
- Malignant peripheral nerve sheath tumour
- Melanotic schwannoma
- Neurofibroma
- Perineurioma
- Schwannoma
-
The sellar region is at the base of the brain, near the pituitary gland. Due to their position, tumours that grow here are often associated with vision and growth problems.
- Granular cell tumour of the sellar region
- Pituicytoma
- Spindle cell oncocytoma
Support and Information Services
Research & Clinical Trials Information
You can also join our active online community.
In this section
Get support
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading
- Common types of childhood brain tumour
- Common types of adult brain tumour
- Common symptoms of a brain tumour in children
- Common symptoms of a brain tumour in adults
- How brain tumours are diagnosed
- Treatment for childhood brain tumours
- Treatment for adult brain tumours
- Brain tumour research we’re funding
- Living with a brain tumour
Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.